 “Interfacing costs? They’re too high.”
“Interfacing costs? They’re too high.”
We hear that a lot. The cost is frustrating, especially to physicians who need to implement EMRs for Meaningful Use. First there are the license fees. Then you find out you need an interface. Or two. Or six. That number can expand with the interoperability requirements in Meaningful Use Stage 2.
Software Packages vs. Software Programs
Here’s why I think interfacing costs are frustrating. After 30 years of PC use and now BYOD smartphones and tablets, we’re used to thinking in terms of software packages and applications. Think Office 2010 for business productivity. A nice little set of apps on your Android phone. Even cloud applications like Salesforce are basically software packages. They’re (mostly) intuitive. They work (more or less) out of the box.
What we have in healthcare IT are programs, not packages.
EMRs and related systems are software programs that must be configured. Workflows have to change in order to get value out of the software. The programs must be enticed to play well together and accurately communicate the information they harbor to those that need it, when they need it. Rinse and repeat for every application, clinical or otherwise, that you need to integrate.
So let’s break down the costs. When you buy an EMR, you buy the hardware, licenses, maintenance, implementation, and training. It takes time to get the EMR up and running. It’s not plug and play. Rinse and repeat for every application, clinical or otherwise, that you need to integrate.
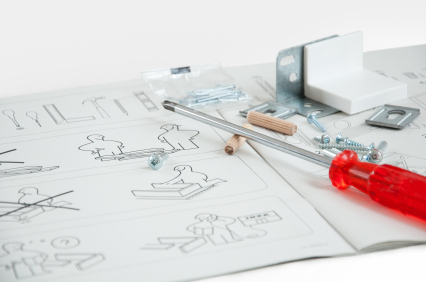
Ikea vs. a Custom Wood Shop
Here’s another way to approach the costs. It’s like thinking you’re buying your furniture from Ikea (some assembly required), but in reality you’re working with a Maine craftsman in a custom wood shop. We’re still in the custom wood shop stage with healthcare IT. You might have the wood all dried and ready to plane, you might have some basic designs to leaf through in a catalog, but there are still a thousand decisions to make. Wood stain, upholstery, seating style… that’s just the beginning. Even then, once the furniture is built if you don’t take care of it, make sure there is enough humidity in your environment, it just might crack.
You’d think that because an EMR vendor had interfaced with a lab system run by ten other clients, the vendor would just copy their interfacing code and reuse it with their next client. But that’s not how it works. Because we lack standards, because we’re dealing with complex data, because the delivery of care is complex – because of all these things, sharing that data is complex. As the volume of data increases and regulatory compliance demands interoperability and security, that complexity rapidly grows.
If we break down the costs of interfacing, there’s an enormous amount of custom work. It’s not uncommon to spend upwards of 40 hours just on coding an interface. And gap analysis? Days of intricate HL7 pipe- counting. Testing? Are you working with real de-id’ed data so you know your validation cycle is clean? Or will you be picking through code searching for needles in that haystack as you watch your project timeline go down the drain and costs rise just to get it done? That’s the environment that the EMR vendor’s analysts and developers are facing.
This sounds like an apology for high prices and charging-just-because-we-can. But the reality is: this is the state of our industry. Personally, I think we can do better. If we can turn interfacing and interoperability into a viable commodity – if we can drive down the cost, imagine what we could do in healthcare.
Where Should Interfacing and Interoperability Go?
Tell us some of your answers to this question. Where does your experience, knowledge and creative imagination take you?
